Introduction
Burnout among physical therapists (PTs) is a significant concern that manifests as emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. This phenomenon not only affects the therapists' health but also compromises the quality of patient care and the overall effectiveness of the healthcare system.1 Research indicates that a substantial percentage of PTs experience burnout at various stages of their careers, with estimates suggesting that nearly half of PTs report feelings of burnout, comparable to rates observed in other healthcare professionals such as physicians and nurses.2,3 The implications of burnout extend beyond individual therapists, as it can lead to increased turnover rates, thereby straining healthcare resources and impacting patient safety.4,5
Understanding Burnout
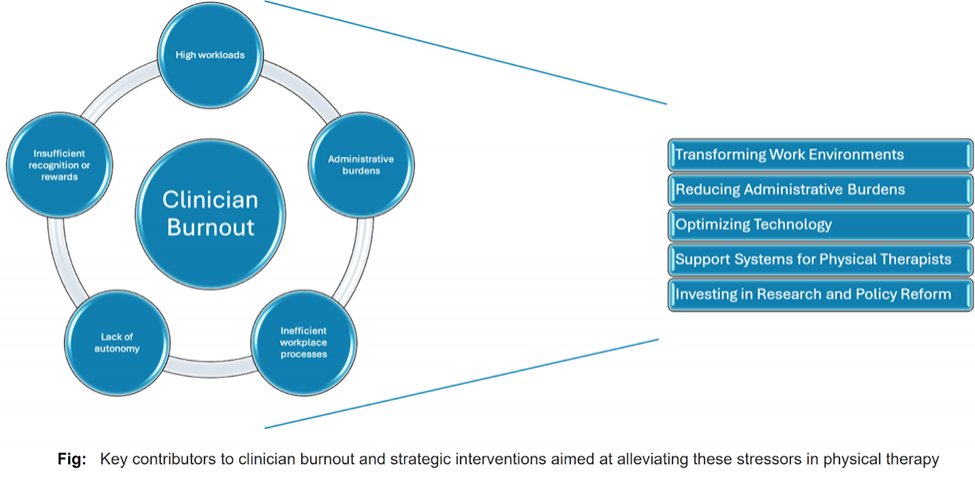
Understanding the multifaceted nature of burnout in physical therapists requires exploring systemic, organizational, and individual factors.6 High workloads, administrative burdens, inefficient workplace processes, lack of autonomy in clinical decision-making, and insufficient recognition or rewards for patient care efforts are frequently cited as primary stressors. For instance, PTs often express frustration with the bureaucratic demands of documentation, insurance claims, and compliance with regulatory standards, which can detract from their clinical responsibilities.4,5,7 Additionally, the physically demanding nature of PT work, characterized by long hours of standing and manual therapy, exacerbates both physical and mental fatigue, contributing to significant professional dissatisfaction.2 This dissatisfaction can lead to a decline in the quality of patient care, as therapists may become disengaged and less effective in their roles.1,4
Transforming Work Environments
Transforming the work environment for PTs is essential in mitigating burnout. This transformation can involve reassessing patient loads and the physical demands placed on therapists, such as the number of patients seen daily and the physical effort required for each session. Enhancing interprofessional collaboration, particularly with occupational and speech-language therapists, is especially beneficial in a team-based approach for patients with neurological conditions, facilitating a more balanced workload distribution and improving the overall quality of patient care.8 Further, fostering a workplace culture that prioritizes work-life balance, continuous feedback, and recognition is crucial for sustaining a positive work environment.7 While leadership within PT organizations often provides resources to mitigate these stressors, the key challenge remains ensuring that therapists effectively receive and utilize this support.9 Additionally, it is worth noting that members who are well-connected within these organizations are more likely to feel supported and less prone to burnout.10
Reducing Administrative Burdens
Reducing administrative burden is another critical strategy to combat burnout among PTs. Streamlining documentation processes and simplifying billing practices can alleviate the pressures associated with administrative tasks.1 For instance, using integrated EHR systems that automatically populate billing fields can minimize redundant data entry and reduce errors. However, it is important to address the potential for less thorough documentation that could result from over-reliance on automation.2,11 Additionally, advocating for clearer reimbursement processes and hiring dedicated administrative staff can allow PTs to concentrate on patient care, enhancing job satisfaction and reducing burnout.2,5,11
Optimizing Technology
The effective use of technology can significantly reduce burnout by improving clinical efficiency and allowing physical therapists to concentrate more on patient care. Advanced software solutions can automate routine tasks, such as scheduling and patient communications, freeing up therapists to focus on direct patient interactions.11,12 For instance, well-designed Electronic Health Records (EHRs) streamline documentation, ensuring compliance with regulatory standards while minimizing administrative burdens. These systems often include built-in templates and prompts for common treatment protocols, which aid less experienced therapists in maintaining accurate records while offering customizable features that allow seasoned practitioners to input data and access patient histories quickly. EHRs have been shown to reduce clinician stress and burnout by prioritizing patient-centered care over paperwork, underscoring the critical role of user-friendly technology in healthcare.11
Support Systems for Physical Therapists
Building robust support systems for physical therapists involves creating a culture that normalizes seeking help and mental health support. Providing access to mental health resources, such as professional counseling and stress management programs, can be invaluable in addressing the psychological needs of therapists.9 Peer support groups and discussion forums can offer spaces for PTs to share experiences and strategies for managing job-related challenges, fostering a sense of community, and reducing feelings of isolation.2,3 Workshops focused on physical self-care, including ergonomic techniques and exercises to mitigate physical wear and tear, are also critical in promoting therapist well-being.5 Also, professional development opportunities that keep clinicians updated on the latest practices can enhance their competence and confidence, contributing to job satisfaction and reducing burnout.2,9
Investing in Research and Policy Reform
Investing in research and policy reform is essential to address burnout among physical therapists comprehensively. Securing funding for studies exploring the impact of various work environments on clinicians’ health can guide the development of effective policies and practices to enhance job satisfaction and reduce burnout rates.2,5 For example, advocating for mandatory breaks and flexible scheduling options can help prevent physical overexertion and promote long-term career sustainability. Additionally, reforms focusing on better compensation models rewarding quality of care rather than quantity can alleviate the pressure of excessive caseloads, allowing therapists to prioritize delivering optimal patient outcomes.9
Summary
Addressing clinician burnout among physical therapists necessitates a multifaceted approach that emphasizes systemic changes rather than relying solely on individual resilience. By transforming work environments, reducing administrative burdens, optimizing technology, enhancing support systems, and advocating for policy reforms, we can create a sustainable healthcare system that supports its most valuable asset—its clinicians (Figure 1). The integration of these strategies is essential not only for the well-being of physical therapists but also for the overall effectiveness and safety of patient care within the healthcare system. Key Words: clinician well-being, healthcare system reform, systemic transformation.
References
- Hall L, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PloS One. 2016;11(7):e0159015. doi:10.1371/journal.pone.0159015
- Burri SD, Smyrk KM, Melegy MS, et al. Risk Factors Associated With Physical Therapist Burnout: A Systematic Review. Physiotherapy. 2022;116:9-24. doi:10.1016/j.physio.2022.01.005
- Pugliese M. Mentorship and Self-Efficacy Are Associated With Lower Burnout in Physical Therapists in the United States: A Cross-Sectional Survey Study. J Educ Eval Health Prof. 2023;20:27. doi:10.3352/jeehp.2023.20.27
- Ferguson JJ, Fritsch A, Rentmeester C, Clewley D, Young JL. Feeling Exhausted: How Outpatient Physical Therapists Perceive and Manage Job Stressors. Musculoskeletal Care. 2023;21(3):845-855. doi:10.1002/msc.1761
- Cakirpaloglu SD. Strain and Serenity: Exploring the Interplay of Stress, Burnout, and Well-Being Among Healthcare Professionals. Frontiers in Psychology. 2024;15doi:10.3389/fpsyg.2024.1415996
- National Academies of Sciences, Engineering, and Medicine. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. The National Academies Press; 2019:334.
- Goldberg DG. “Anxiety, COVID, Burnout and Now Depression”: A Qualitative Study of Primary Care Clinicians’ Perceptions of Burnout. J Gen Intern Med. 2023;39(8):1317-1323. doi:10.1007/s11606-023-08536-2
- Ikeda K, Sasada S. Development of a New Scale for the Measurement of Interprofessional Collaboration Among Occupational Therapists, Physical Therapists and Speech-Language Therapists. Hong Kong J Occup Ther. 2022;35(2):146-153. doi:10.1177/15691861221111439
- Wei H, Roberts P, Strickler J, Corbett RW. Nurse Leaders’ Strategies to Foster Nurse Resilience. J Nurs Manag. 2019;27(4):681-687. doi:10.1111/jonm.12736
- Luo D, Song Y, Cai X, et al. Nurse Managers' Burnout and Organizational Support: The Serial Mediating Role of Leadership and Resilience. J Nur Manage. 2022;30(8):4251-4261. doi:10.1111/jonm.13852
- Kroth PJ, Morioka-Douglas N, Veres S, et al. Association of Electronic Health Record Design and Use Factors With Clinician Stress and Burnout. JAMA Netw Open. 2019;2(8):e199609. doi:10.1001/jamanetworkopen.2019.9609
- Kruse CS, Mileski M, Dray G, Johnson Z, Shaw C, Shirodkar H. Physician Burnout and the Electronic Health Record Leading Up to and During the First Year of COVID-19: Systematic Review. J Med Internet Res. 2022;24(3):e36200. doi:10.2196/36200
The author declares no competing interests.
Author Bio:
Dr. Tarang K. Jain, PT, DPT, PhD is an Associate Professor at Northern Arizona University in the Department of Physical Therapy and Athletic Training. With a career spanning 20 years in orthopedic and sports physical therapy, Dr. Jain holds a transitional Doctor of Physical Therapy (t-DPT) and PhD in Rehabilitation Sciences from the University of Kansas Medical Center, Kansas City, KS. He has actively contributed to the Academy of Orthopaedic Physical Therapy by co-authoring the 'Screening for Orthopaedics' monograph and participating in various committees. His research primarily focuses on biomechanical movement analysis and the neural control of movement, particularly studying chronic ankle instability to develop effective rehabilitation strategies. Dr. Jain is also committed to mentoring, playing a pivotal role in the professional development of his students and peers.